The Evan Group have published a major paper on lung cancer in the journal Cell.
Lung cancer is currently the third most common cancer in the UK, with over 46,000 new diagnoses every year. Additionally, lung cancer is the most common cause of UK cancer death, accounting for 22% in 2014, which equates to around 100 deaths from the disease every day. Although improvements in cancer prevention, detection and treatment have doubled the overall rate of cancer survival in the last 40 years, lung cancer remains a disease with substantial unmet need due to its poor five-year survival rate of just 10%, which has seen little improvement during the last decade. Unfortunately, despite its prevalence and often poor prognosis, lung cancer is also the most preventable form of the disease as 86% of cases can be linked to smoking and 9% to a diet insufficient in fruit and vegetables.1
Although commonly thought of as a single disease, primary lung cancer is actually the term for a group of different cancers that arise from the various cell types within the lungs: Small Cell Lung Cancer (SCLC), fast-growing cancers that normally form in the bronchi near the centre of the chest; and Non-Small Cell Lung Cancer (NSCLC), which accounts for about 87% of UK lung cancers and is itself a class of three cancers that behave and respond to treatment in a similar way. The three types of NSCLC are adenocarcinoma, which forms in the mucus-making cells that line the airways; squamous cell cancer, which begins in the flat cells covering the airway surfaces; and large cell carcinoma, which is identified by its large and round cancerous cells.1
To understand how cancers such as these form, it is often easiest to draw parallels between cells and cars: both rely on correct interplay between countless components in order for them to work properly to complete their various functions. In the case of the car, its primary purpose is transport. This requires the car engine, accelerator and brakes to all work together appropriately for the car to move in a controlled and regulated manner. If the accelerator were to become stuck down, or if the brakes were to fail, driving would be uncontrolled and the results would likely be disastrous. For cells, one of their essential functions is their ability to grow and divide. In parallel to driving, this process also requires an 'engine' (formed from cellular structures), with proteins taking the roles of 'accelerators' (oncogene proteins) and 'brakes' (tumour suppressor proteins) to ensure cells grow and divide in a controlled and regulated way. If oncogenes become permanently switched on or if there is too much of them, and/or if tumour suppressor proteins become permanently switched off or if there is too little of them, it results in uncontrolled cell growth and division; a prominent hallmark of cancer.
Since the early 1980s, two oncogene proteins, Ras and Myc, have been known to cooperate to drive tumour formation, with both implicated in NSCLC. KRas, one of the three Ras family members, is thought to be mutated in and to be a cause of ~30% of NSCLCs, particularly in smokers, whilst abnormally high amounts of Myc protein are found in over 70% of NSCLCs.2-4 Initial research has determined multiple methods through which KRas and Myc can drive cell growth and division: they jointly promote production of cell cycle proteins (the 'engine' driving growth),5-7 Myc overcomes Ras-controlled cell growth arrest,8-9 and Ras prevents Myc-induced cell death.8,10 The exact molecular mechanism that allows KRas and Myc to cooperate in driving tumorigenesis has, however, remained unclear.
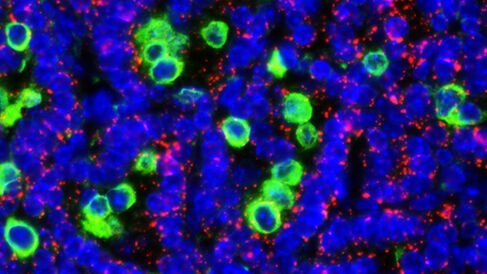
In their new paper, Kortlever et al. explore the contribution of Myc to the evolution and progression of mutant KRas NSCLCs. They find that mutant KRas results in the slow formation of benign adenomas that rarely evolve into aggressive NSCLC. It is only when there is sustained co-activation of Myc, alongside mutant KRas, that adenomas dramatically progress to invasive and lethal adenocarcinomas. Use of a 'switchable genetics' drug-mediated activation system (MycERT2), where tamoxifen treatment causes rapid activation of Myc in the epithelium of KRas adenomas, shows that Myc induces the signalling protein IL-23 to stimulate efflux of B, T and NK lymphocytes (removal of these immune system cells enhances tumour cell survival). In parallel Myc induces another signalling protein, CCL9 (a chemical attractant known as a chemokine), to promote recruitment of macrophages to the epithelium. Through consequently enhanced VEGF signalling, macrophages in turn promote angiogenesis and vasculature remodelling, giving the tumour cells an increased blood and oxygen supply for survival. Importantly, deactivation of Myc through the MycERT2 system resulted in rapid regression of the tumours; macrophages exited the tumour and the vasculature returned to normal discrete vessels, whilst B, T and NK lymphocytes repopulated the tumour mass leading to tumour cell death. Using this switchable genetics approach, the authors have uncovered a previously unappreciated manipulation of the immune system by oncogene proteins in tumours, and have identified two signalling molecules responsible for the resulting lung cancer progression.
In speaking about the implications of this research, lead author Dr Kortlever commented that "Cancer immunotherapy can be very successful but has its limitations and is mainly focussed on boosting the adaptive immune system of a patient. The finding that innate immunity is directly and critically regulated by an oncogenic engine of cancer progression is a new paradigm that may greatly expand our approach to immunotherapy."
1Cancer Research UK website. Accessed November 2017.
2Land et al., Nature304:596 (1983).
3Rodenhuis et al., Cancer Res.48:5738 (1988).
4Richardson and Johnson, Semin. Oncol.20:105 (1993).
5Born et al., Mol. Cell. Biol.14:5710 (1994).
6Leone et al., Nature387:422 (1997).
7Wang et al., Cell Cycle10:57 (2011).
8Evan and Littlewood, Science281:1317 (1998).
9Vaque et al., J. Biol. Chem. 280:1112 (2005).
10Tsuneoka and Mekada, Oncogene19:115 (2000).
